Medicare Advantage (MA) enrollment has grown at a rapid pace over the last few years, and the share of eligible Medicare beneficiaries enrolled in MA now stands at 48 percent. As of January 2023, almost 30.7 million people are enrolled in MA plans.
As enrollments in MA plans have surged, so too have the complaints about inappropriate marketing tactics and other issues. The Centers for Medicare & Medicaid Services (CMS) reported that Medicare beneficiary complaints about MA marketing more than doubled between 2020 and 2021. In response, CMS issued a final rule in 2022 that included rules for increased consumer protections. A Senate Finance Committee investigation in late 2022 corroborated CMS findings and made several policy recommendations to CMS for better addressing these issues.
In this three-part series, we will look at how conversational AI and automation can help healthcare payors and Third-Party Marketing Organizations (TPMO) improve agents’ sales performance and drive better conversions, ensure compliance to CMS rules for MA marketing, and reduce churn by understanding each beneficiary’s need holistically.
Driving Higher Medicare Advantage Conversion with Conversational AI and Automation
Medicare Advantage enrollment continued at a rapid pace in 2023, adding more than 2.7 million beneficiaries. For healthcare payors and TPMOs supporting the enrollment, this meant adding thousands of temporary workers to handle the volume of incoming leads during the Annual Enrollment Period (AEP). Healthcare payors and TPMOs go through this motion every year. In the first part of this three-part series, we will discuss how conversational AI and automation can help these organizations improve sales agents’ performance and drive better conversions.
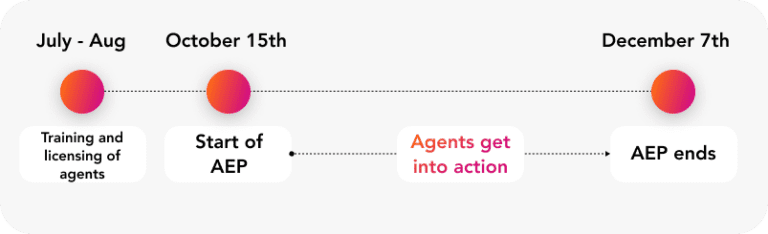
Every year, leading up to the start of the Annual Enrollment Period (AEP) in October, payors and TPMOs initiate a process of recruiting and training personnel and getting them licensed and ready for AEP. Once the AEP starts on October 15, the floodgates open and agents get into action, promptly addressing incoming leads and striving for maximum conversions. This continues until December 7, when AEP comes to an end. During the AEP, leads come in at a relentless pace, making it very difficult to course correct and make changes to lead handling and the enrollment process.
Uniphore analysis shows that the top 5 percent of sales agents are 20x better than the bottom 30 percent. What if you could analyze the winning behaviors of your top agents, understand what works and roll out these winning behaviors throughout your entire agent population by coaching them in real-time? It is easier said than done.
Typically, all organizations use some kind of quality scoresheet to analyze their agent calls and understand how their agents are performing. However, there are two problems with this analysis: first, most organizations do a random sample (typically 2-4 calls per agent per week), and second, these calls are scored manually, which is time consuming, and therefore introduces a lag between when the call is completed to when a call is scored. QA teams have a tough task on their hand to make an impact on improving sales performance because insights are obtained in a delayed timeframe across a large number of parameters, which make it difficult to roll out any changes across large number of agents.
Maximize agent performance with insights, not instincts
With conversational AI, QA teams can monitor 100 percent of the calls, on same day, for compliance and for agent performance across call handling, listening, communication skills, etc. Analyzing 100 percent of the calls allows QA teams to get insights into the performance of leaders and laggards in the team across different conversational behaviors and compare the skills where leaders score higher. Conversational AI can provide detailed analysis of key speech elements normalized by call segments and identify the conversational behaviors that drive better sales conversion across the top agent population—something that was previously not possible.
Rapidly operationalize winning behaviors at scale
Generating insights into behaviors that drive better conversion is just the first part of the puzzle. To truly maximize conversions, these insights need to be implemented across the agent population. Since AEP spans only 53 days and incoming lead volumes are very high, it is often difficult to take agents off live calls for training. Typically, suggestions to improve performance are disseminated and may be discussed during start-of-day huddles. However, this does not institutionalize the behavioral change that is needed.


Operations teams can also quickly test hypotheses with a sample agent population by conducting A/B analysis and rapidly roll out successful hypotheses to all agents.
Improve the quality of leads, increase your chances of conversion
As AEP attracts a large volume of incoming leads, it is inevitable that a considerable portion of these leads are either not eligible for MA plans or they may not align to focus areas for the insurer or TPMO. To address this, conversational AI-powered voice bots with a light touch approach can swiftly gather information from callers and assess the incoming leads to identify high-quality prospects for agent engagement. Care must be taken while designing these conversations to ensure that the experience is positive for the caller and that the lead is qualified with minimal back and forth.
Conversational AI and automation can be a game changer for MA enrollment as it allows organizations to learn from the conversational behaviors of top performers and it applies the learning across the entire workforce. This could mean an improvement in performance of up to 20 percent more enrollments per agent for the bottom-performing agent population. When applied across the agent population, this can substantially impact the sales performance of these organizations.
